Spider Veins Overview
What Is a Spider Vein?
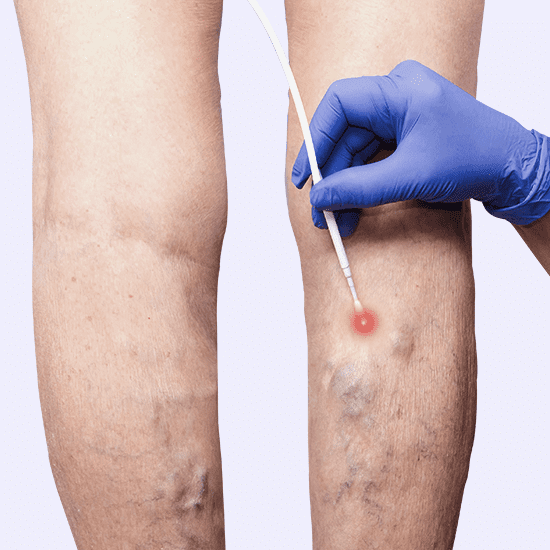
Spider veins (also known as telangiectasias) are tiny, unhealthy blood vessels that develop close to the surface of the skin. They’re commonly found on the legs or face, and they can be blue, red, or purple. Their thin, thread-like appearance and clustered formation resemble a spider web, which is how their name was derived. Spider veins might represent a deeper issue called chronic venous insufficiency, or they might only cause superficial damage.
What Causes Patients to Visit Spider Vein Clinics?
Impaired circulation is behind most spider veins. Many patients have a structural abnormality in their vein, such as a broken valve, that disrupts proper blood flow. When a venous valve isn’t working correctly, veins encounter collection or reflux (backflow) of blood, which exerts pressure on venous walls. Rather than traveling to the heart, the blood pools or heads toward your feet, which causes bulging in the vein area below the valve. That pressure prompts new, defective veins to take form and branch out from the troubled vein. Those spindly branches are the spider veins you see. Some people are bothered by spider veins physically, if they present symptoms like bleeding, cramping, swelling, or heaviness, particularly after long stretches of sitting or standing. Other people are only bothered by them visually, since they can be asymptomatic. Roughly 50% of Americans have either spider veins or varicose veins. However, spider vein causation is underdiagnosed and undertreated. Your spider veins might be harmless, or they might be associated with a disease. Visit California Vein Clinic to see what’s causing your spider veins.
Who Gets Spider Veins?
Since aging influences spider vein formation, they’re more common in adults. Genetic predisposition is the greatest predictor of telangiectasias, raising your odds to nearly 100% if your biological parents both have spider veins. Elevated estrogen levels also contribute to their formation, so women are at higher risk. Some additional risk factors are distinctly female, such as pregnancy, hormone therapy, and birth control usage. However, other factors impact both genders, like leg injuries, blood clots, prior vein surgery, obesity, and jobs that require a lot of sitting or standing.
What Are the Reasons Behind Spider Veins?
Some patients view spider veins as an unavoidable side effect of aging. But the primary culprit is usually chronic venous insufficiency. This vein disease can and should be treated to relieve pressure on your veins. Otherwise, spider veins will continue to form, even if you treat them cosmetically. Your vein system runs deeper than the veins you see beneath your skin. Tackling the structural issues in deeper veins will prevent those defective surface veins from developing.
What Symptoms Require a Visit to a Vein Clinic in California?
Your spider veins might not cause symptoms, or you might not realize the correlation of symptoms. For example, if your legs feel heavy and swollen at the end of your work shift, or you have eczema or dermatitis near a spider vein, you might not draw a connection. But symptoms like these, as well as stinging, tingling, burning, cramping, and Restless Legs Syndrome are all tied to spider veins. Some patients experience severe ulceration and discoloration as a result of spider veins. Whether you have no symptoms, serious symptoms, or seemingly unrelated symptoms, it’s wise to visit California Vein Clinic for a venous assessment.
How Does California Vein Clinic Treat Spider Veins?
Our vein clinics in San Diego and San Jose won’t suggest spider vein treatments you don’t need. If you don’t have venous insufficiency or vein disease, but dislike your spider veins, we’ll offer aesthetic solutions like sclerotherapy. If your problem is more serious, we have a broad range of methods to treat the visibility and symptoms of spider veins, as well as the diseases that cause them. Visit our board certified vein specialists in California to ensure that the veins, the symptoms, and the cause are all thoroughly addressed.
What’s the #1 Vein Treatment for Spider Veins?
Spider veins are frustratingly common, but luckily, they’re also safe and simple to treat. The best treatment depends on your unique circumstances, which must be analyzed through a comprehensive physical examination and additional testing, if needed. Don’t agree to spider vein treatment if a vein doctor doesn’t first check for venous insufficiency. Otherwise, they’re wasting your time and money and might miss a serious health issue that demands attention.
Foam or Liquid Sclerotherapy:
California Vein Clinic views this treatment as a first line of therapy for superficial spider veins. Our doctors inject an “irritant” into the vein to scar it shut, which closes the faulty pathway and sends blood into healthy veins. For deeper veins, sclerotherapy is sometimes combined with mechanical ablation administered by a catheter.

Endоvеnоuѕ Lаѕеr Ablation:
This injection procedure also targets venous insufficiency, in addition to the appearance of spider veins. It’s a superior tactic to vein stripping surgery, since it’s outpatient and only uses local anesthetics. However, it causes a bit more bruising and discomfort after treatment than radiofrequency ablation does.
Endovenous RF Ablation:
Radiofrequency ablation is a top treatment for spider veins, especially those that result from chronic venous insufficiency. This technique heats the vein walls with thermal energy from high frequency soundwaves, which causes them to collapse. The vein is no longer viable, so blood re-routes into veins that can pump it to your heart.

Laser Treatment:
Endovenous lasers, described above, inject the vein, treating both veins and vein disease. In contrast, superficial laser treatment is done at the skin’s surface with tools like pulsed dye lasers, so it doesn’t treat venous insufficiency. It works for smaller veins, not the larger, more bulbous veins, and occasionally is used in conjunction with other methods like sclerotherapy. The pain perception is higher with lasers, and it’s not advised for patients with certain skin sensitivities.

Compression Stockings:
Many patients ask about compression stockings, and certain insurance companies recommend a trial of them before other procedures. Support stockings apply steady pressure to your legs, which helps veins pump blood to your heart. This only works if the compression stockings are the right size and don’t roll at the top. It’s important to note that compression stockings help blood flow with symptoms like swelling, but they don’t change the appearance of spider veins or treat vein disease or faulty valves.

Physical Activity:
The more we move, the more our leg muscles contract, helping veins transport blood against the gravitational pull. Circulation and symptoms improve with daily exercise (it won’t eliminate existing veins). Changing positions is key, since simply standing increases vein pressure, just like sitting does. If your career calls for extensive sitting or standing (ie: teachers, pilots, hosts, drivers, surgeons, data specialists), it’s important to squeeze exercise in, particularly if you have vein disease. If you don’t have time for a full workout, try lunges or squats by your desk, walking while teaching, flexing calf muscles while driving or flying, or climbing stairs between meetings. Also, elevate your legs above your heart while at rest.

